Is Retatrutide ketosis in a vial?
TL;DR: A lot of drugs try to mimic the benefits of ketogenic diets, and Retatrutide might be the closest yet.
Nutritional Ketosis Mimetics
I've long been interested in pharmacalogical interventions that attempt to do what a ketogenic diet does (and amused or at least bemused by the apparent zeal and lack of concern by their advocates in contrast to the horror reserved for nutritional ketosis). Because a ketogenic metabolism (KM) entails a complete metabolic state, these interventions almost always involve stimulating or blocking some pathways that then replicate some end-state marker present in a KM, while leaving other pathways in glucose mode. Whether remaining in this kind of metabolic mixed state for long periods is healthful is an open question, and probably depends on the exact intervention.
Probably the most famous of these kinds of intervention is Metformin, which may work in part by inhibiting Complex I [1], and hence carbohydrate metabolism at the point of the electron transport chain. In this category, I have previously only deeply researched and personally experimented with:
- Exogenous ketones
- IV NAD+
- DNP (2,4-dinitrophenol)
- Bremelanotide (note, this may not actually be a ketosis mimetic)
As per my usual, I have intended to write long posts summarising the research and on-the-ground anecdotes on each of them, but life hasn't allowed it.
Retatrutide: GLP-1 agonist with an interesting twist
Retatrutide is an iteration on GLP-1 agonists. Like tirzepatide, it adds to this by also being a GIP agonist, but goes still further to a third action: it stimulates glucagon receptors. The previous generation of these I have not been terribly interested in, because it seemed to me that their primary mechanisms of action had to do with falsely signalling satiety, something I'm not a big fan of.
[Note: after I wrote this line, but before finishing this post, Gary Taubes wrote on exactly this, arguing that in fact tirzepatide itself already works by fuel partitioning [2]! So retatrutide, with its glucagon receptor activity may simply be another supporting mechanism in that direction, rather than completely different.]
At worst that would lead to all the problems of caloric restriction I have written on before, especially loss of lean mass and metabolic slowdown. Lots of people report fatigue on semaglutide and tirzepatide, and high risk of muscle loss has been discussed as well. That said, I have a few friends on these who have gotten good results where other methods done in good faith failed. Power to them, especially since they lift heavy and take care of that muscle mass!
But glucagon receptor activation would presumably approach the fat loss problem from the other side of the equation, the spontaneous fat loss side of the equation, by stimulating fatty acid oxidation. In fact, it has been shown to increase energy expenditure in mice [3]. Moreover, glucagon receptor activation would mimic a lower insulin-to-glucagon ratio, as would retatrutide's insulin lowering effect [4]. Insofar as this is true, one might expect it to act like a ketogenic diet without the carbohydrate restriction. Lo and behold, retatrutide increases ketogenesis.
Retatrutide increases ketogenesis?
What got my attention was seeing this claim with the below graphic somewhere on Twitter or Reddit.
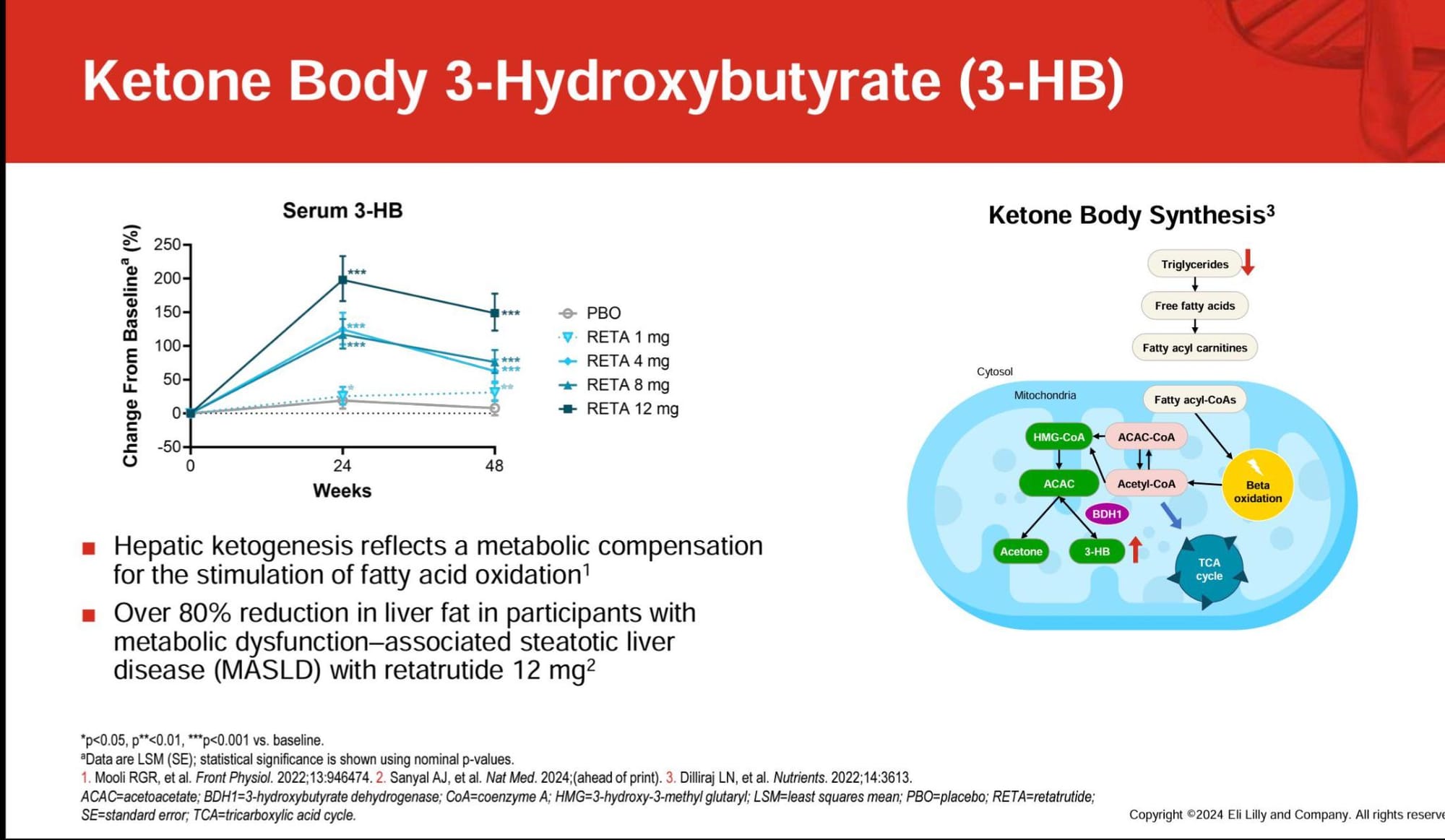
I have not discovered the true origin of this image [update, origin found! My guess was correct, more in footnote] , but I'm guessing it's a slide from one of the researchers at/for Eli Lilly, presenting on the paper in citation 2 [4]. Let's look at that paper.
Retatrutide causes ketogenesis AND it's considered a Good Thing?
Well, yes, as long as ketogenesis doesn't come from carb restriction, it's perfectly fine! (wink)
The point of this paper is to show that subjects on Retatrutide are cured of fatty liver, and it is noted that the higher the ketogenesis, the more effective the cure.
You and I already know that ketogenic diets effectively treat NAFLD (Nonalcoholic fatty liver disease, now renamed to MASLD, metabolic dysfunction-associated steatotic liver disease, presumably to further distance the condition from alcoholism?) [4]. But now we can do it with an injection, and when we do, there is ketogenesis.
But is it really a lot of ketogenesis?
The table and the graph derived from it show only the increase of β-hydroxybutyrate relative to baseline. And they use mg/dL. Are they trying to make it look more ketogenic than it is? To put it in more familiar terms, here is the data in mmol, in absolute terms.
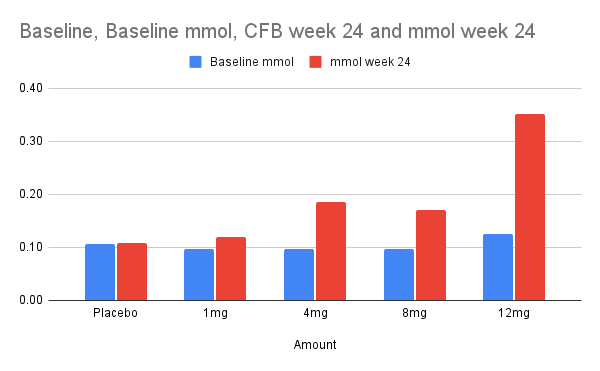
So... Sure, the highest dose more than doubled serum BOHB. And that made for a level that is... still below clinically defined ketosis. It's still interesting, but it's not "Reta puts you in ketosis!" interesting.
On the other hand, these are measurements at 24 weeks. When I alerted r/Retatrudtide that I was writing this post and seeking some anecdotes, one correspondant, u/SubParMarioBro, told me that he thinks that those reporting a high energy response to retatrutide (many but not all--some report fatigue, which I'll come back to later) probably experienced pharmacalogical ketosis that eventually subsided. One reason he thinks this is, that when he subsequently took exogenous ketones, he got a strikingly familiar energetic sensation. So his hypothesis is that the researchers may have missed peak levels by waiting 24 weeks before measuring. In addition to that, I had another responder tell me that her bloodwork showed ketosis despite a high carb diet.
So, I am not excluding the possibility that retatrutide is more ketogenic initially than later, and that this is more common than the researchers themselves may realise.
Does retatrutide enhance keto-adaptation?
One aspect that makes this more plausible is that stimulating glucagon receptors would be expected to cause endogenous glucose production from liver glycogen, hence depleting it. Anecdotally, some Redditors have complained that they "hit a wall" quicker on reta and need to supplement carbs more diligently before workouts. This would be consistent with retatrutide initiating keto-adaptation, since liver glycogen depletion is the main keto-adaptation bottleneck. Other consistent indications include oft-cited need for electrolytes to combat fatigue and muscle cramps.
So for regular people who are on high carb diets, it seems plausible that retatrutide pushes them toward keto-adaptation, which would EITHER keep them perpetually in a keto-flu-like situation that requires electrolytes and is characterised by fatigue and the constant need to refill glycogen with carbs, OR if people instead cut carbs intentionally or incidentally, it could hasten keto-adaptation and put them squarely in ketosis.
So what if you're on a ketogenic diet already?
That's a good question. Glad you asked. I don't think we know. However, in the most recent trial the researchers have apparently now added a ketoacidosis warning. (Sorry for the image cutoff. I'm not in this trial and it's not my image, I just took the photo from social media.)
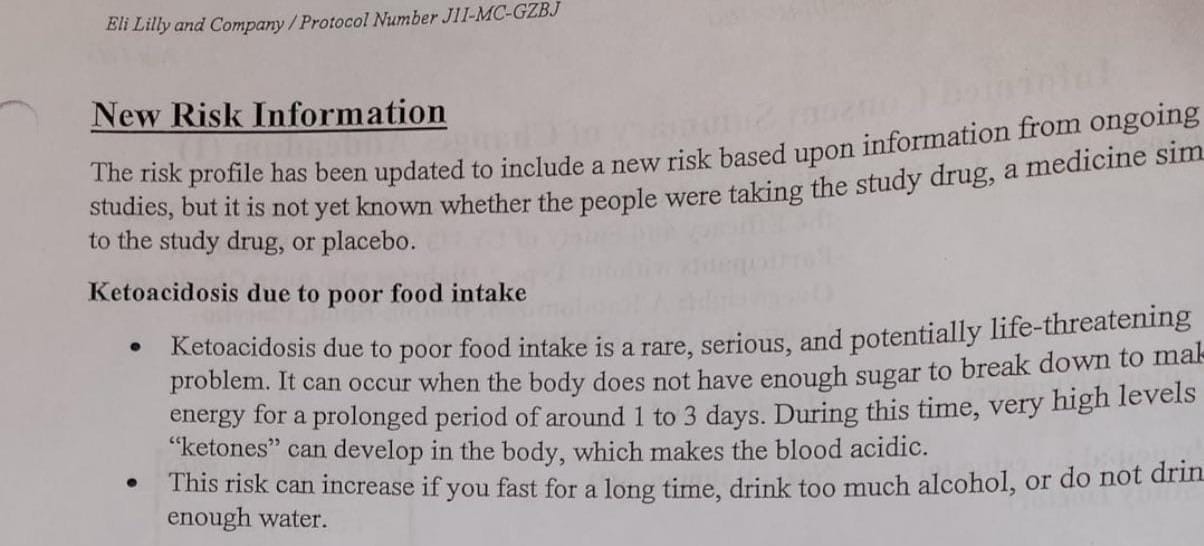
I'm not sure what to make of this, actually. Is it just a CYA because they know "ketones" will rise? Are the researchers that noted higher BOHB celebrating ketogenesis or not? As far as I can tell there have been no reports of ketoacidosis occurring in Retatrutide trials, although there are case reports from tirzepatide [5]. One Redditor suggests that they may have observed new adverse events on retatrutide from an ongoing trial that hasn't been reported on yet, which I suppose is possible.
Definitely most people on social media seem to be interpreting this as "Don't do low carb on reta." But as far as I can tell many people are in fact doing a ketogenic diet while on retatrutide with no adverse effects. My expectation is that they would be synergistic.
Footnotes and References
1 Fontaine, Eric. “Metformin-Induced Mitochondrial Complex I Inhibition: Facts, Uncertainties, and Consequences.” Frontiers in Endocrinology 9 (December 17, 2018): 753. https://doi.org/10.3389/fendo.2018.00753.
2 Taubes, Gary. “Why Do We Lose Weight on GLP-1 Drugs?” Substack newsletter. Uncertainty Principles (blog), April 24, 2025. https://uncertaintyprinciples.substack.com/p/why-do-we-lose-weight-on-glp-1-drugs.
3 Coskun, Tamer, Shweta Urva, William C. Roell, Hongchang Qu, Corina Loghin, Julie S. Moyers, Libbey S. O’Farrell, et al. “LY3437943, a Novel Triple Glucagon, GIP, and GLP-1 Receptor Agonist for Glycemic Control and Weight Loss: From Discovery to Clinical Proof of Concept.” Cell Metabolism 34, no. 9 (September 6, 2022): 1234-1247.e9. https://doi.org/10.1016/j.cmet.2022.07.013.
4 Sanyal, Arun J., Lee M. Kaplan, Juan P. Frias, Bram Brouwers, Qiwei Wu, Melissa K. Thomas, Charles Harris, et al. “Triple Hormone Receptor Agonist Retatrutide for Metabolic Dysfunction-Associated Steatotic Liver Disease: A Randomized Phase 2a Trial.” Nature Medicine 30, no. 7 (2024): 2037–48. https://doi.org/10.1038/s41591-024-03018-2.
Treatment with retatrutide improved several markers of insulin resistance at 24 and 48 weeks, with greater changes at week 48 (Table 2). Fasting serum insulin concentrations were reduced at week 48 compared with baseline by up to 70.9% with retatrutide treatment (P < 0.01 versus placebo, doses 4 mg or greater). Serum C-peptide concentrations were reduced by up to 50.5% with retatrutide at 48 weeks (P < 0.001 versus placebo, 8 mg or greater). Significant improvements in Homeostatic Model Assessment for Insulin Resistance (HOMA2-IR) computed with fasting insulin were observed with retatrutide doses of 4 mg or greater, with changes up to −69.3% at 48 weeks (P < 0.001 versus placebo). Similarly, at 48 weeks HOMA2-IR computed with fasting C-peptide significantly improved with the 8 mg and 12 mg doses with changes up to −54.5% (Table 2; P < 0.001 versus placebo).
4 There are three citations listed.
-
The first is the source of the statement "Hepatic ketogenesis reflects a metabolic compensation for the stimulation of fatty acid oxidation" from Emerging Role of Hepatic Ketogenesis in Fatty Liver Disease.
That's a weird way to state it. In fact the original quote is "The speculation from these observations is that hepatic ketogenesis reflects a metabolic compensation for the increased delivery of fatty acid to the liver, helping to offload the hepatic fat", attributed to another author writing on de novo lipogenesis. I don't think the primary evolutionary function of ketogenesis is to offload excess liver fat, but I agree it reflects that effect. -
The second citation is the meat here. It is the origin of the data in the graph of β-hydroxybutyrate responses on Retatrutide and it is the same paper cited in [3]
-
The third is just credit for the ketone body synthesis description from The Evolution of Ketosis: Potential Impact on Clinical Conditions, although that paper does not contain that graphic, so perhaps the slide creator made it.
Update about the origin:
You can't find that BHB info because Lilly posted it at a conference last year but now it's gone for some reason. I saved it as a pdf. Here's the full poster. You can also find more BHB data on their MAFLD phase 2 published data. https://t.co/TAo7hfAry6 pic.twitter.com/81IGgLd4s2
— FlexNP (@rn_flex) May 4, 2025
Here is the original poster presentation, thanks to @rn_flex
4 Mardinoglu, Adil, Hao Wu, Elias Bjornson, Cheng Zhang, Antti Hakkarainen, Sari M. Räsänen, Sunjae Lee, et al. “An Integrated Understanding of the Rapid Metabolic Benefits of a Carbohydrate-Restricted Diet on Hepatic Steatosis in Humans.” Cell Metabolism 27, no. 3 (March 2018): 559-571.e5. https://doi.org/10.1016/j.cmet.2018.01.005.
5 Ou, Yingyong, Zhiwei Cui, Siyu Lou, Chengyu Zhu, Junyou Chen, Linmei Zhou, Ruizhen Zhao, Li Wang, and Fan Zou. “Analysis of Tirzepatide in the US FDA Adverse Event Reporting System (FAERS): A Focus on Overall Patient Population and Sex-Specific Subgroups.” Frontiers in Pharmacology 15 (November 6, 2024). https://doi.org/10.3389/fphar.2024.1463657.
